We found 53 results for EFM
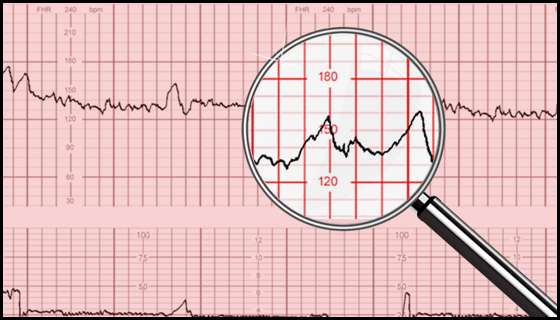
EFM Case Study #16: Equipment Interpretation Failure
Perinatal clinicians are frequently unaware of the equipment limitations they use routinely. Non-invasive blood pressure machines, pulse oximeters, electronic fetal monitors, and the human that use them, are fallible. Understanding how a piece of equipment works, anticipating limitations under certain clinical conditions, and then modifying care is necessary for a patient’s safety. Over reliance on equipment breeds errors and increases malpractice risk.
.png?access_token=4PqCEj5SaAizvuww2i34dqWcySFaWL2XVKKkhB0H)
EFM Case Study #17: Oxytocin - Myths & Truths
This activity evaluates the serious implications of oxytocin misuse by busting oxytocin myths with current scientific facts. The truth about how to properly administer oxytocin safely and effectively is evaluated with support from evidence-based resources.
EFM Case Study #18: Hypertensive Crisis & Stroke
Preeclampsia and any other form of hypertension make a stroke six- to nine-times more likely to happen. Stroke and the hypertensive crisis that may precede it are medical emergencies requiring treatment within 30-60 minutes of onset yet proper management is delayed or lacking; this increases medical-malpractice risk. This case study examines the current recommendations for the management of acute-onset severe hypertension in pregnancy.
EFM Case Study #19 & #20: Influence of SUD on EFM
When a pregnant patient misuses or becomes dependent on any addictive substance during pregnancy, two people are exposed: the pregnant patient, and the fetus/newborn. It is estimated that approximately 5% to 7% of pregnant persons use addictive substances. Among these, approximately 21% report misuse, 27% identify the need or desire to decrease or stop their use, and approximately 32% do not receive provider counseling of how their substance use could affect their infant. This activity will present a case study of SUD in pregnancy, highlighting the recognizable EFM changes along with strategies to address the effects.
EFM Case Study #21: Failure to Monitor
Failing to maintain a continuous EFM strip can imply that the perinatal team was inattentive to the mother, fetus, or both. This activity discusses how failing to monitor the FHR/UC data violates the standard of care for the reasonably prudent obstetrical caregiver and offers solutions to prevent it.
EFM Case Study #22: Intermittent Auscultation Safety and Risks
There is a current disconnect between scientific evidence that supports the use of intermittent auscultation (IA) in low-risk pregnant patients and the use of IA in clinical practice. This activity outlines strategies to providers and hospitals on how to safely adopt IA into clinical practice.
.png?access_token=4PqCEj5SaAizvuww2i34dqWcySFaWL2XVKKkhB0H)
EFM Fundamentals in Practice #01: UC Data, Part 1
Attainment and ongoing maintenance of electronic fetal monitoring (EFM) skills is a requirement of all perinatal practitioners who actively participate in the care of pregnant patients. This module in the series concentrates on uterine contraction data especially related to frequency, duration, intensity, and resting tone.
.png?access_token=4PqCEj5SaAizvuww2i34dqWcySFaWL2XVKKkhB0H)
EFM Fundamentals in Practice #02: UC Data, Part 2
Attainment and ongoing maintenance of electronic fetal monitoring (EFM) skills is a requirement of all perinatal practitioners who actively participate in the care of pregnant patients. This module in the series concentrates on UC data especially related to abnormal uterine contraction patterns that are frequently seen during labor and the evaluation and calculation of Montevideo units.
.png?access_token=4PqCEj5SaAizvuww2i34dqWcySFaWL2XVKKkhB0H)
EFM Fundamentals in Practice #03: FHR Data, Part 1
Attainment and ongoing maintenance of electronic fetal monitoring (EFM) skills is a requirement of all perinatal practitioners who actively participate in the care of pregnant patients. This module in the series concentrates on the assessment and interpretation of baseline fetal heart rate data.
.png?access_token=4PqCEj5SaAizvuww2i34dqWcySFaWL2XVKKkhB0H)
EFM Fundamentals in Practice #04: FHR Data, Part 2
Attainment and ongoing maintenance of electronic fetal monitoring (EFM) skills is a requirement of all perinatal practitioners who actively participate in the care of pregnant patients. This module in the series concentrates on the assessment and interpretation of fetal heart rate data especially detecting the presence of accelerations and periodic or episodic decelerations.
.png?access_token=4PqCEj5SaAizvuww2i34dqWcySFaWL2XVKKkhB0H)
EFM Fundamentals in Practice #05: Maternal-Fetal Oxygenation
Attainment and ongoing maintenance of electronic fetal monitoring (EFM) skills is a requirement of all perinatal practitioners who actively participate in the care of pregnant patients. This module in the series concentrates on maternal-fetal oxygenation and acid-base balance.
.png?access_token=4PqCEj5SaAizvuww2i34dqWcySFaWL2XVKKkhB0H)
EFM Fundamentals in Practice #06: 3-Tier FHR Interpretation System
Attainment and ongoing maintenance of electronic fetal monitoring (EFM) skills is a requirement of all perinatal practitioners who actively participate in the care of pregnant patients. This module in the series concentrates on concepts regarding the application of oxygen physiology to the NICHD 3-Tier FHR Interpretation Category System.
.png?access_token=4PqCEj5SaAizvuww2i34dqWcySFaWL2XVKKkhB0H)
EFM Fundamentals in Practice #07: General Interventions
Attainment and ongoing maintenance of electronic fetal monitoring (EFM) skills is a requirement of all perinatal practitioners who actively participate in the care of pregnant patients. This course in the series concentrates on the general interventions that are administered in an effort to gain more information about the maternal-fetal condition.
.png?access_token=4PqCEj5SaAizvuww2i34dqWcySFaWL2XVKKkhB0H)
EFM Fundamentals in Practice #08: Interventions To Reduce Uterine Activity
Attainment and ongoing maintenance of electronic fetal monitoring (EFM) skills is a requirement of all perinatal practitioners who actively participate in the care of pregnant patients. This module in the series concentrates on the interventions that are administered in an effort to reduce uterine activity.
.png?access_token=4PqCEj5SaAizvuww2i34dqWcySFaWL2XVKKkhB0H)
EFM Fundamentals in Practice #09: Interventions To Promote Fetal Oxygenation
Attainment and ongoing maintenance of electronic fetal monitoring (EFM) skills is a requirement of all perinatal practitioners who actively participate in the care of pregnant patients. This module in the series concentrates on the interventions that are administered in an effort to promote fetal oxygenation.
We found 3 results for EFM
-
Education
Section: MI Public Website -
Assessments
Section: MI Public Website -
Course Packages
Section: MI Public Website

